In a retrospective comparative cohort study, Hou et al. 1) published in the American Journal of Translational Research, the authors—affiliated with the Department of Oncology, Department of Gynaecology and Obstetrics, and Department of Neurosurgery at Shijiazhuang People’s Hospital (Hebei, China), as well as Beijing Water Conservancy Hospital—compared the survival benefit and safety profile of lenvatinib versus donafenib as conversion therapy in patients with hepatocellular carcinoma (HCC) at China National Liver Cancer (CNLC) stages I–III.
Lenvatinib demonstrated significantly superior survival outcomes—both in overall survival and progression-free survival—compared to donafenib. It also showed better tolerability, with fewer grade ≥3 adverse events.
❌ 1. Study Design: Retrospective = Weak Evidence
This is yet another retrospective single-center analysis, plagued by inherent biases—selection, reporting, and confounding—that no amount of statistical massaging can resolve. No randomization, no blinding, and no control for treatment timing or physician discretion. In oncology, where treatment nuances matter, such designs should be considered hypothesis-generating at best, not guidance for clinical practice.
📉 2. Sample Size: Statistically Thin, Clinically Hollow
The study included only 76 patients (40 lenvatinib vs. 36 donafenib). Such a low-powered cohort raises major concerns:
PFS difference (4.6 vs. 2.9 months), though statistically significant, is barely clinically relevant.
ORR difference (15% vs. 5.6%) is not even statistically significant (P=0.551) — but still emphasized in the discussion as if it mattered.
Multivariate analysis with such a small dataset is mathematically questionable and likely overfitted.
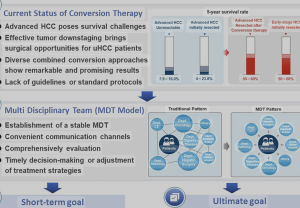
🧱 3. Conversion Therapy? Or Rebranding a Failure?
The term “conversion therapy” is misleading here. These drugs were administered in the hope of downstaging HCC — yet no actual conversion to surgery or local treatment is reported. The authors exploit a term that evokes curative intent without backing it up. This is not conversion therapy — it’s systemic palliation repackaged in euphemism.
🔬 4. Outcome Inflation: OS vs. PFS Discrepancy
While OS doubled (14.9 vs. 7.9 months, P=0.010), PFS barely improved by 6 weeks (4.6 vs. 2.9 months). This disparity suggests that post-progression treatments may have confounded OS — but the study gives no data on subsequent lines of therapy, making the OS benefit unverifiable and potentially misleading.
⚠️ 5. Safety Reporting: Cherry-Picking by Omission
The claim that lenvatinib is “more tolerated” is based on selective listing of fewer grade ≥3 events. But the paper:
Doesn’t define how adverse events were graded.
Doesn’t give the absolute rates of common toxicities (hypertension, proteinuria).
Doesn’t report dose adjustments, interruptions, or treatment duration.
This paints an incomplete and biased picture of safety — likely underpowered to detect real toxicity differences.
🧪 6. Biomarker Analysis: Statistical Necromancy
Hazard ratios for AFP and hepatic vein invasion are presented as independent prognostic factors. However, these are well-established predictors and add nothing novel to the study. Worse: interpreting these from a cohort of 76 patients with multiple covariates is statistical overreach bordering on negligence.
🏥 7. Institutional Echo Chamber
All four departments involved belong to one hospital. No external validation, no multicenter inclusion. The study reflects local practice, local bias, and perhaps local drug availability policies — not generalizable conclusions for global hepatology or oncology communities.
🤯 Final Verdict
This is a fragile, underpowered, and poorly contextualized study that tries to extract clinical meaning from statistical noise. It overstates the benefits of lenvatinib, mislabels its purpose as “conversion therapy,” and cherry-picks safety data — all wrapped in the false authority of multivariate modeling over 76 patients.
Calling this “evidence” is dangerous.
Using it to guide therapy is reckless.
🧠 Takeaway Message from the Study for a Neurosurgeon
Although this study focuses on systemic therapy for hepatocellular carcinoma (HCC), a neurosurgeon—especially one involved in neuro-oncology or metastatic brain disease—can extract the following key message:
Systemic therapies like lenvatinib may extend survival modestly in solid tumors such as HCC, but their actual impact on neurosurgical decision-making (e.g., eligibility for resection of brain metastases or control of neurological symptoms) remains indirect, unmeasured, and largely speculative.
⚠️ Critical Insight: The study uses the term “conversion therapy” without demonstrating any actual conversion to surgery, which is a red flag for neurosurgeons who base treatment on resectability and local disease control.
Such papers illustrate the growing pressure to rebrand palliative systemic treatments as potentially curative, despite limited supporting evidence—highlighting the need for neurosurgeons to remain critical readers and decision-makers when systemic therapies are proposed in multidisciplinary settings.
Hou Y, Gao Z, Han Y, Liu C, Su X, Zhang D. Comparison of survival benefit and safety profile between lenvatinib and donafenib as conversion therapy in patients with hepatocellular carcinoma. Am J Transl Res. 2025 May 15;17(5):3496–3504. doi: 10.62347/PBLA2928. PMID: 40535653; PMCID: PMC12170375.