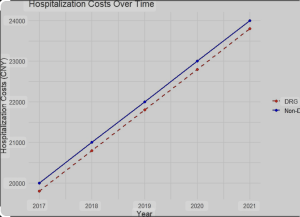
In a retrospective observational econometric analysis Luo et al. from the Panzhihua Central Hospital, Sichuan Provincial People’s Hospital, Chengdu, Sichuan, China 1) in Frontiers in Public Health attempt to quantify the cost-containment effects of DRG-based payment systems in China hospitals using advanced statistical tools. They claim significant cost reductions (especially in drug and material expenditures) and more “concentrated” cost distribution post-reform.
Major Criticisms
1. **Shallow Econometric Sophistication Masquerading as Rigor**
While Propensity Score Matching (PSM) and Difference-in-Differences (DiD) models are commonly used to infer causal effects, their validity hinges on critical assumptions — none of which are addressed with sufficient care here. The authors provide no robustness checks, falsification tests, or sensitivity analyses. The technical glitter hides conceptual rust.
2. **Missing Clinical and Institutional Variables**
The model assumes that cost differences arise solely from the payment model shift. However, the study entirely ignores factors such as surgical complexity, comorbidity profiles, institutional practice variations, and physician incentives. This is not just an omission — it’s methodological malpractice when dealing with heterogeneous surgical fields like neurosurgery and cardiothoracic surgery.
3. **No Outcome Metrics Beyond Cost**
The study conflates cost-cutting with success. Nowhere do the authors analyze whether outcomes (e.g., complications, readmissions, mortality) changed after DRG implementation. DRG-induced gaming and “upcoding” are well-documented phenomena — why is this not even mentioned?
4. **Absence of Transparency in Data Access and Integrity**
Administrative datasets from tertiary hospitals in China are not publicly accessible. The authors make no mention of ethical approvals, auditing standards, or data completeness. The lack of transparency undermines credibility and replicability.
5. **Editorial Negligence and Journal Padding**
This paper feels like a policy white paper disguised as peer-reviewed science. There is no clinical insight, no policy nuance, and no attempt to contextualize findings in terms of patient care or system equity. The conclusions are overly optimistic, detached from potential unintended consequences, and presented in the tone of bureaucratic triumphalism.
Definitions of Concern
-
DRG payment reform: A bundled-payment model that may incentivize hospitals to discharge patients prematurely or avoid complex cases.
-
Cost concentration: A euphemism here for reducing variance without exploring whether cost suppression compromises care.
-
Policy recommendation: A performative phrase used without detailed stakeholder analysis or discussion of unintended effects.
Conclusion
This study is the statistical equivalent of a polished brick — heavy in format, hollow in insight. It deploys a shallow econometric toolkit to reach predictable and politically convenient conclusions, conveniently sidestepping the real-world complexity of surgical care in China. That it was accepted in *Frontiers in Public Health* underscores a worrying trend: quantitative noise triumphing over qualitative understanding in modern health policy discourse.
Final verdict: A *low-impact publication* with the intellectual ambition of a government press release. Proceed with skepticism.